Equicare Health: Bridging Gaps and Enhancing Networks of Cancer Care
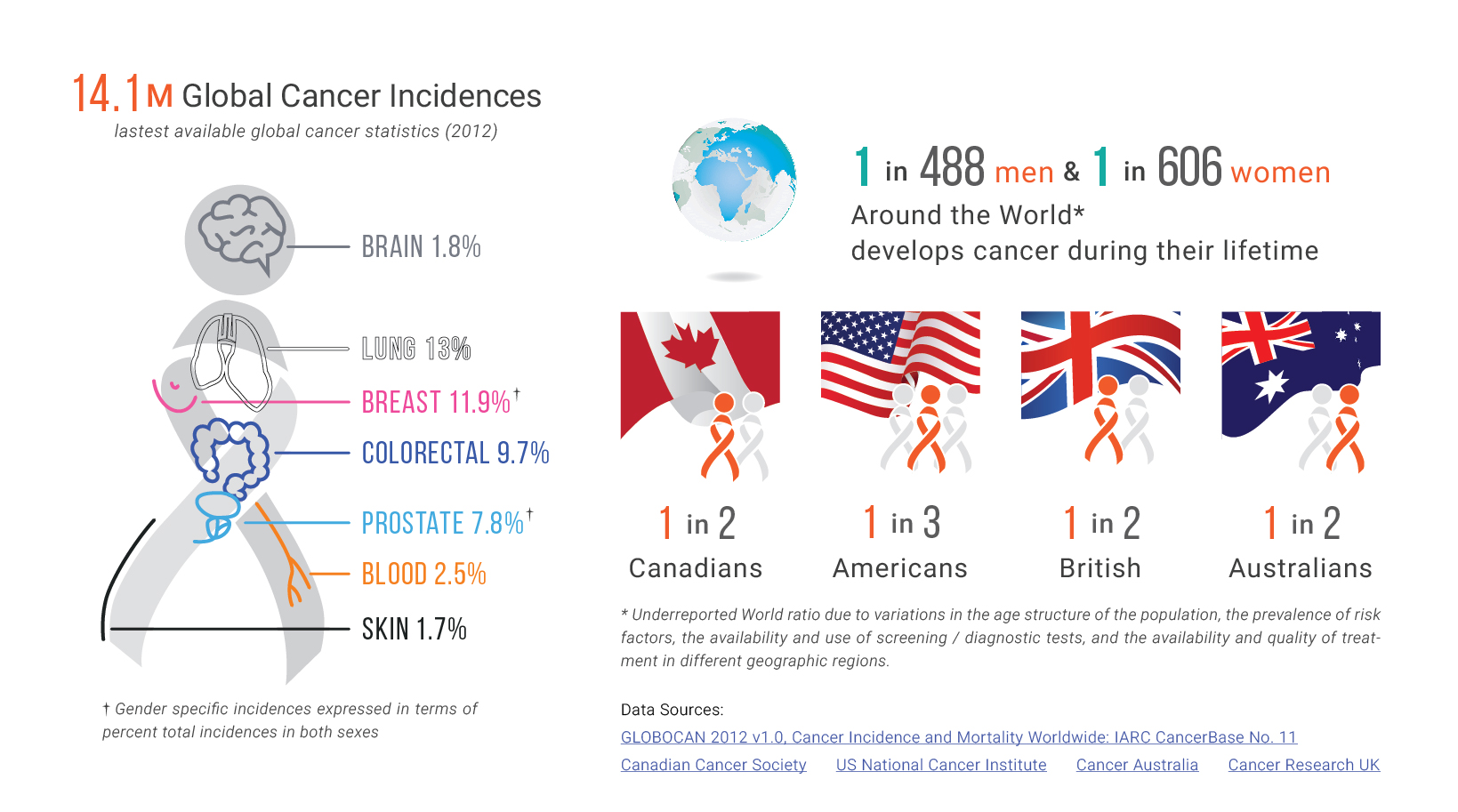
A comprehensive cancer care system encompasses the entire spectrum of care – from prevention and screening to diagnosis, treatment, and survivorship. At the secondary prevention stage, screening is utilized to detect potential cases. At diagnosis, the presence or absence of cancer is confirmed, and the patient is directed to the best course of treatment. Survivorship commences at diagnosis and continues onto long-term survival.
Early detection through cancer screening is paramount to the control and management of cancer cases. Each cancer type has a different screening procedure, making it imperative to understand the different modalities. The differences range in the administration of procedure to its specificity, sensitivity, and unintended consequences.
Once screening procedures are available and accepted, patient engagement initiatives play an important role in helping health professionals attract patients and better tailor treatment plans to specific tumor characteristics. As individuals move through the cancer care continuum – from screening to the stages of care – clear communication and access to education tools improve patient engagement.
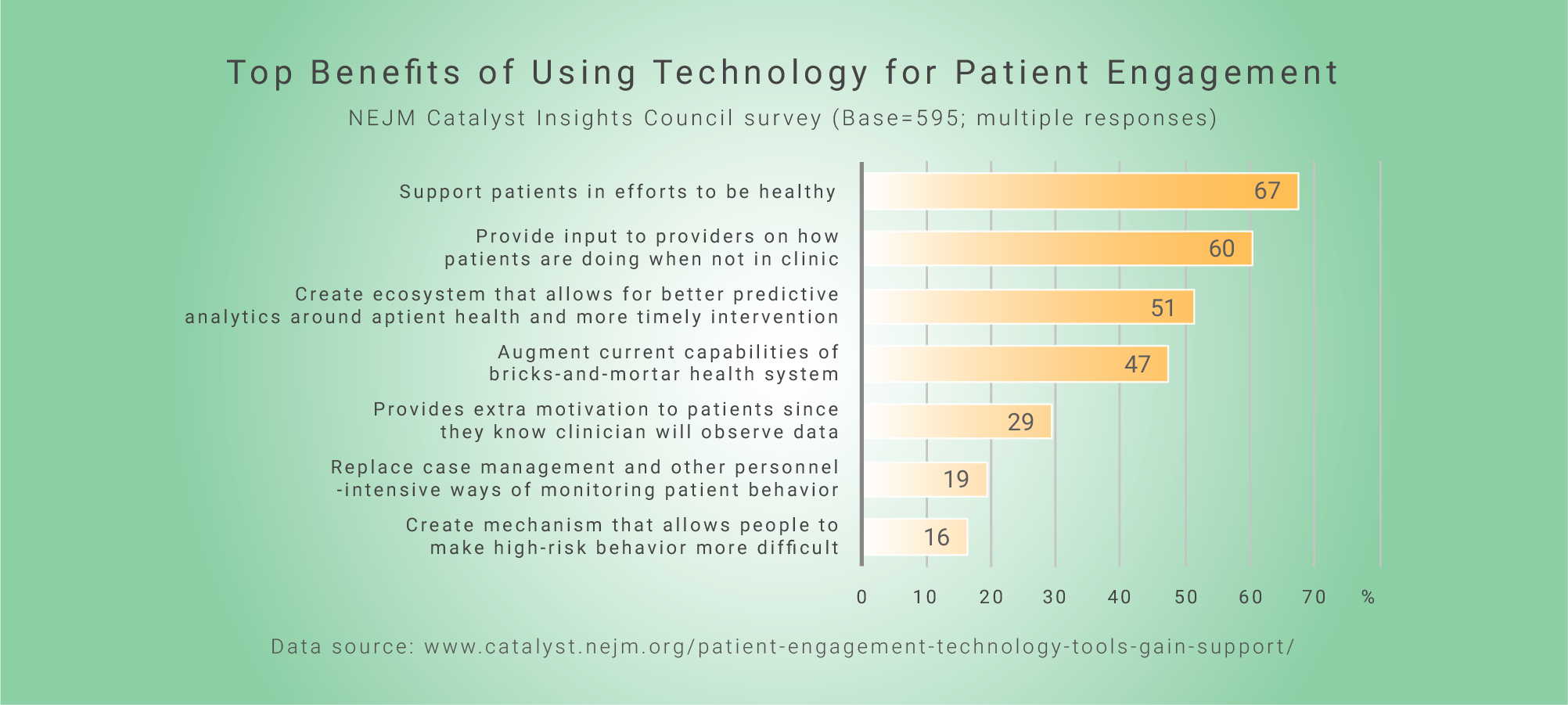
Currently, digital technologies are utilized to enhance engagement with patients, physicians, and allied healthcare professionals by ensuring that accurate information is gathered and transferred throughout the health system in an efficient manner. For instance, patient reported outcomes (PROs) and questionnaires allow self-reporting of symptoms that provide invaluable information for timely risk management and assessing the overall effectiveness of cancer interventions. These tools have proven that enhanced communication and a well-coordinated system is not only advantageous for the patient, but also the medical team, and healthcare system.
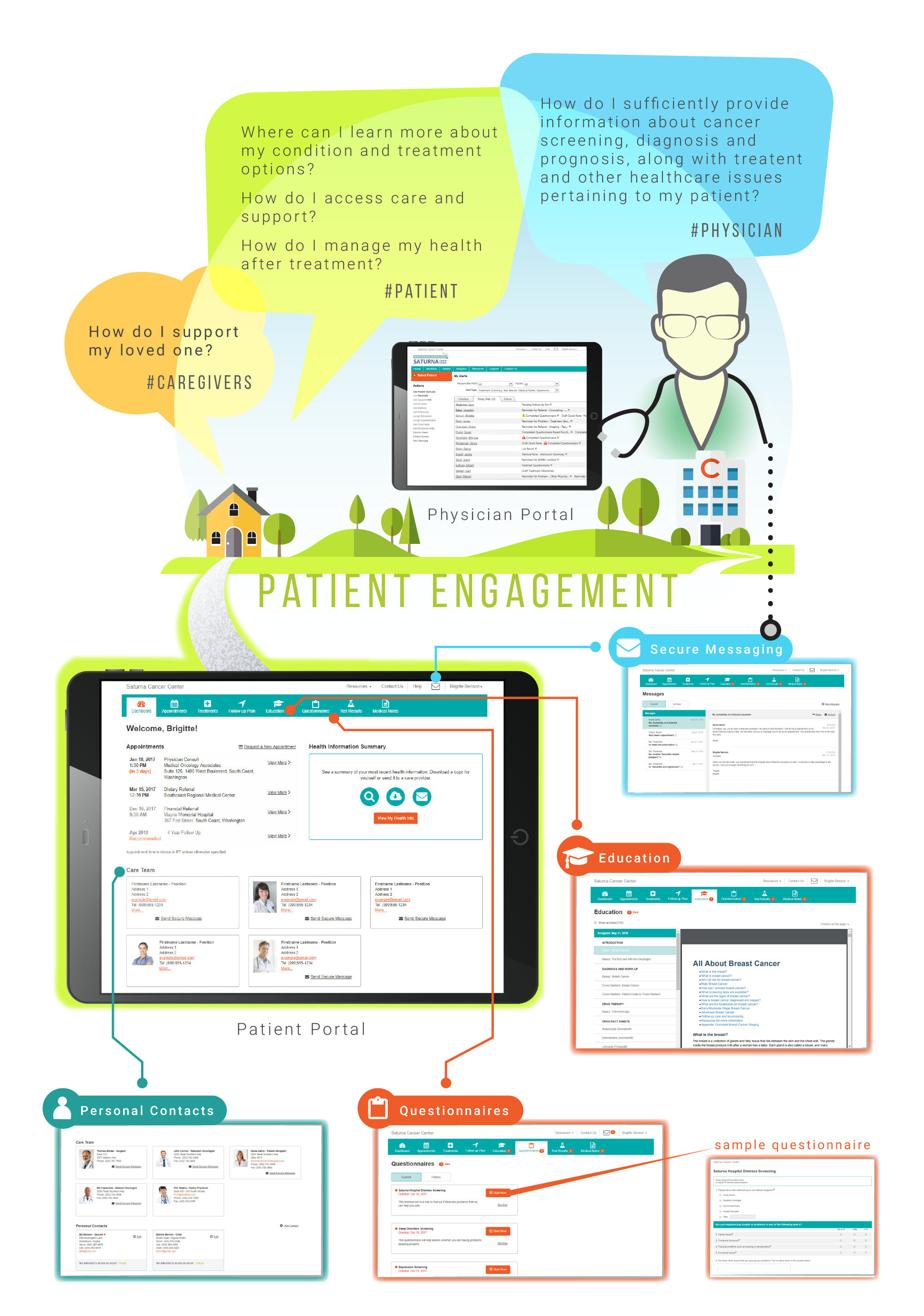
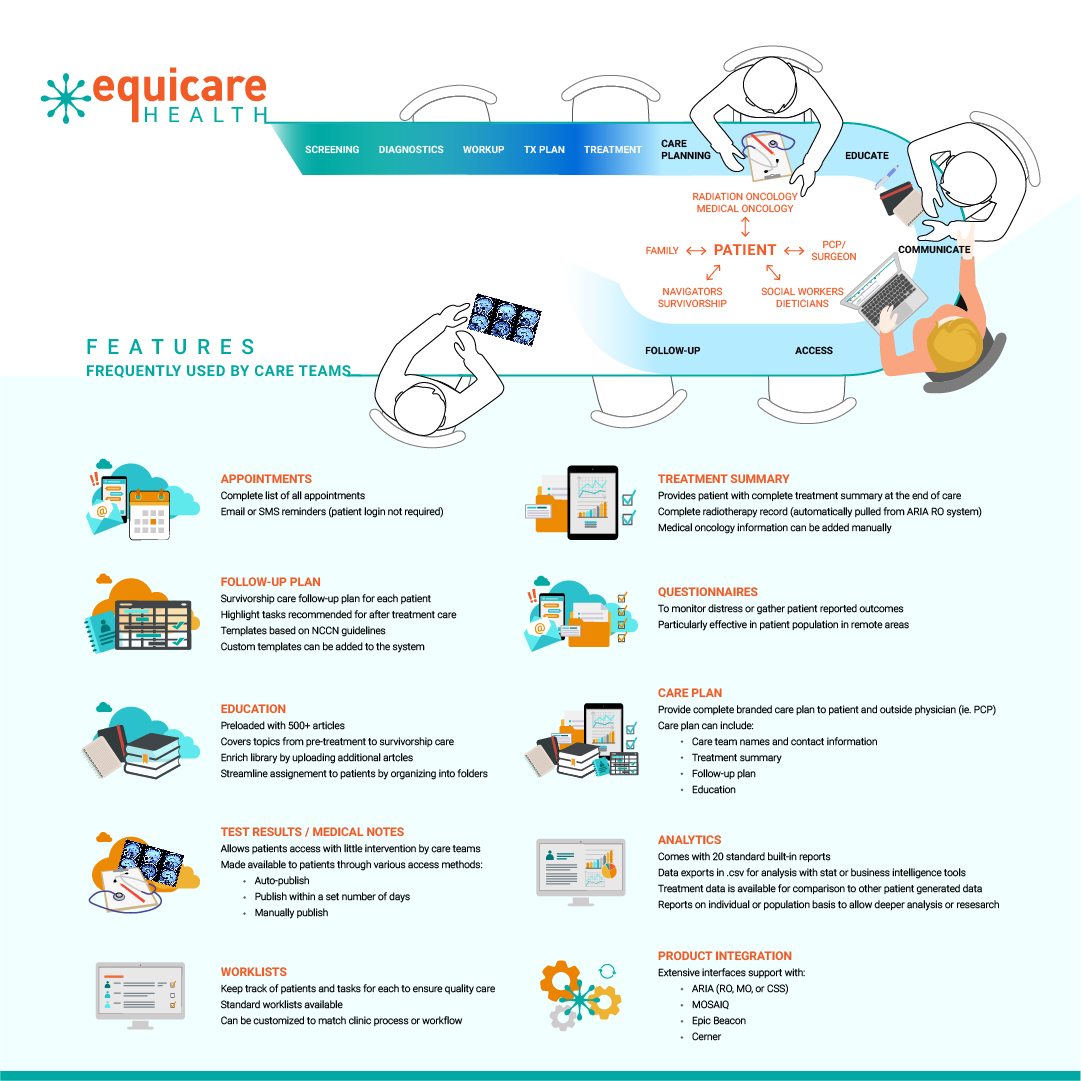
Equicare Health – a leading provider of comprehensive care coordination solutions – aims to assist patients and the medical team through the cancer care continuum. The key is a platform that bridges the gaps and seamlessly connects health professional team members to each other and their patients. For patients, through the patient portal, they can connect with their care team and engage in their healthcare journey. The portal facilitates patient activation and engagement. Once patients receive an invitation letter to sign up, they will be welcomed to Equicare Health’s portal. There, the dashboard guides patients to access resources such as health information, test results, educational material, and appointment schedule. Regular visits to the portal will help patients and their caregivers keep up-to-date on the progress of their treatment and maintain contact with their care team.
The healthcare team enhances patient activation by selecting the appropriate resources available within Equicare CS (ECS). For instance, a physician and/or allied healthcare professional can assign questionnaires to a patient based on the disease site and topic of concern (i.e. depression screening, sleep disorders screening, and/or distress screening). In addition, care teams can assign relevant education covering topics from pre-treatment to survivorship care to assist patients in their own care management. By doing so, patients become actively involved in their own health, and conversations between the care team and the patient are facilitated.
In addition to the care team guiding patients and processing referrals to specialists and health services, they can efficiently coordinate tasks within the care team through Equicare CS. The platform assists with navigation referrals and consults to medical services (i.e. imaging, surgery, radiation oncology), and support services (i.e. counseling, pain management, nutrition, and hospice care). This results in streamlined communication within and between departments and services, making it easier to support patients and enhance the care they need within the many facets of a healthcare team. Once ECS is adequately utilized, patient navigation reports and provider productivity reports can be generated to evaluate quality of care provided to support goals and compliance standards.
The key functionalities of navigation platforms and informatics tools described include the ability to:
1) Do distress management for CoC accreditation
2) Track navigation activity to support the navigator role to administrator
3) Standardize documentation throughout departments
4) Provide timely information to patients
5) Communicate to the entire cancer care team through the platform
Care becomes more difficult during survivorship, as patients are often lost to follow-up or unaware of the heightened health risks that arise post-treatment. This disconnect with the health system proves to be a challenge in managing patients’ medical and psychosocial concerns. Hence, electronic communication tools are imperative to maintaining contact both during and after active care: within the healthcare team and between the team and the patient.
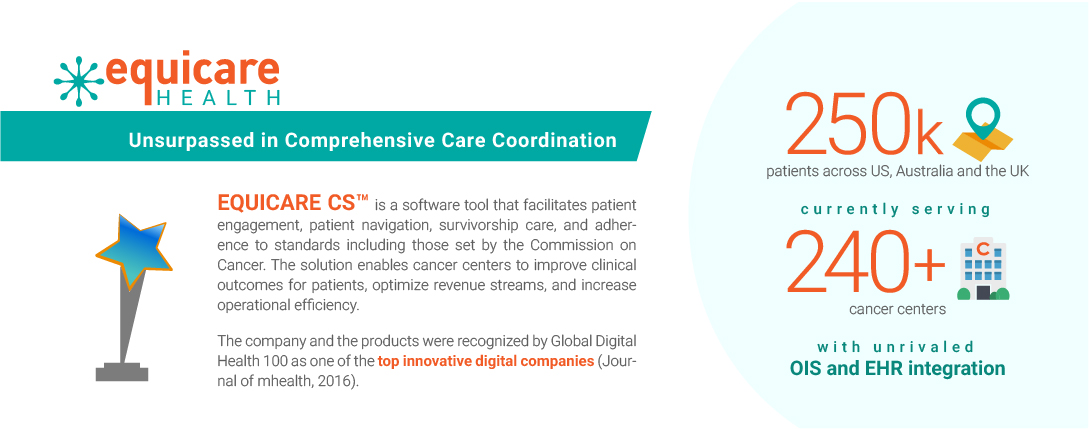
Each step of cancer care is complex and multimodal. There is a need to create a chronic care model to improve clinical outcomes for patients as well as to maximize the operational efficiency for cancer centers. To date, Equicare Health has served over 250,000 oncology patients and 300 cancer centres who continue to utilize the diverse tools that ECS has to offer. With ECS, care coordination and center specific goals are supported through the Service Team and Workflow Specialist at Equicare, who connect with cancer centers and healthcare professionals to assist them in reaching their goals (i.e. number of PROs filled, meeting accreditation standards, and/or enhancing patient engagement). ECS supports patients and healthcare professionals through the care continuum. With its efficient communication tools, tailored educational content, and patient reported outcomes, ECS gathers information, data and education into a comprehensive platform that empowers healthcare providers, patients, and caregivers in the healthcare journey.
Written by Dorri Mahdaviani , who holds a Masters of Public Health (MPH) from the University of British Columbia (UBC). Her academic and professional interests include the areas of chronic illnesses, health care systems and childhood health and development.
Infographics and Design by Ann Wong, who holds a PhD in Biochemistry and Molecular Biology from the Faculty of Medicine at the University of British Columbia (UBC), Canada. She is an author of over 10 SCI publications, having taught at UBC and the Peking University Health Science Center (PUHSC) in Beijing