Diagnostics, workup, and treatment may be complete, but the journey across the cancer care continuum will continue through survivorship management. There are currently over 15 million cancer survivors, and that is to increase to 20.3 million (a 31% increase) by 2026 in the United States alone [1]. In contrast, statistics from about 50 years ago was a count of 3 million survivors in 1971. This dramatic increase is primarily attributed to an aging population, earlier detection, and advanced treatment [2].
The concept of cancer survivorship is not new; it has been over 30 years since Dr. Fitzhugh Mullan described survivorship as a unique phase of cancer care and introduced the idea of “seasons of survivorship. [3]” Since then, this concept has evolved and continues to create some controversy with regards to its exact onset and duration [4]. These can generally be categorized into three categories:
- Phase 1 – acute survival – time from diagnosis to completion of initial treatment
- Phase 2 – extended survival – time from completion of treatment to remission, with careful observations of outcomes from treatments
- Phase 3 – long-term survival
Our focus and attention will be on the period following final treatment and prior to the development of cancer recurrence – long-term survival. Historically, this stage has not been a focus of the care continuum and has several areas of concern, including a less frequent check-in with healthcare providers. Once primary treatment is completed, many patients are often lost to follow-up; are unaware of the heightened health-risks and are ill prepared to manage their medical and psychosocial concerns.
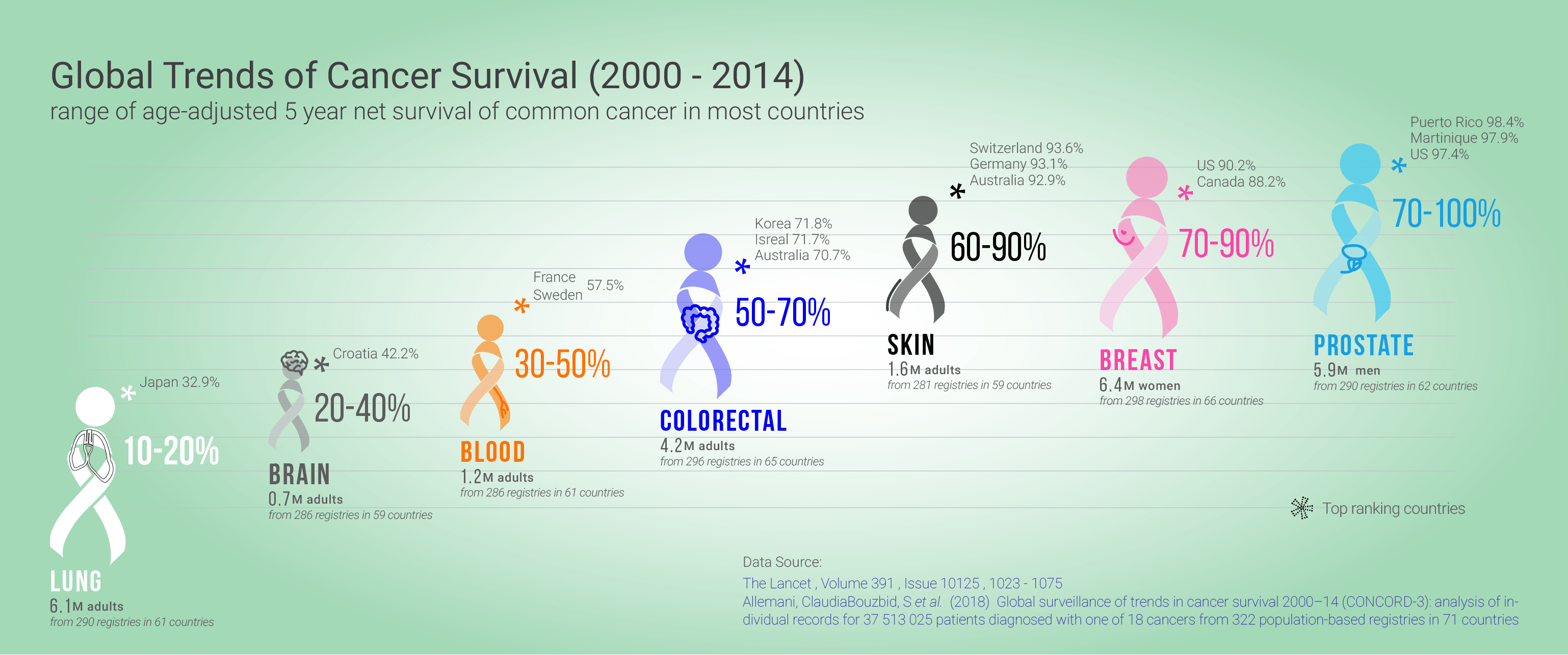
Part of the difficulty with this phase is that it is unique not only for each cancer, but also its various types. For instance, the 5-year survival for breast cancers diagnosed during 2010-2014 is 90.2% in the United States. Its hazard of reoccurrence is highest during the first 5 years at approximately 10%, with the estrogen receptor positive disease maintaining a significant recurrence rate beyond 5 years [5]. For prostate cancers in the United States, the 5-year survival is nearly a 100% [6], with a wide recurrence of 30% – 90% [7]. The high variety of survival rates along with the range of cancer reoccurrence informs the need for tailored surveillance programs.
Follow-up care concerns have become more pertinent in recent years as the new generation of cancer survivors are living longer due to improved access to effective screening, diagnosis, and treatment initiatives. Consequently, the health care delivery system is looking at solutions to efficiently and effectively navigate the long-term and late effects of cancer care as well as other chronic conditions, while taking into account the demands for patient-centered quality of care across the cancer care continuum.
The transition from active treatment to post-treatment care is a critical period for maintaining and enhancing long-term individual and population health. Evidence-based strategies need to be implemented across health systems to ensure that optimal health outcomes are met. Quality of care during survivorship is dependent on essential components of care, as well as ease of access to comprehensive and coordinated care.
Cancer survivorship encompasses:
- Prevention through screening of new and recurrent cancers
- Surveillance of cancer recurrence
- Monitoring of medical and psychosocial late-effects, incorporating interventions for intended and unintended consequences of cancer treatment
- Coordination of care between health professionals to ensure that all the health needs of survivors are met
In order to deliver optimal cancer survivorship care, fundamental changes are needed to ensure that all survivors receive care that is safe, timely, effective, efficient, patient-centred, and equitable. Leading health care systems foster and embrace the creation of an infrastructure to support evidence-based practices. In a world that is complex and continuously enhancing, leading health care systems utilize information technology to better assist health care professionals and patients with cancer care navigation.
Written by Dorri Mahdaviani , who holds a Masters of Public Health (MPH) from the University of British Columbia (UBC). Her academic and professional interests include the areas of chronic illnesses, health care systems and childhood health and development.
Infographics and Design by Ann Wong, who holds a PhD in Biochemistry and Molecular Biology from the Faculty of Medicine at the University of British Columbia (UBC), Canada. She is an author of over 10 SCI publications, having taught at UBC and the Peking University Health Science Center (PUHSC) in Beijing