Cancer is not just one disease, it encompasses many variations of disease. The term cancer is commonly used for diseases where abnormal cells divide in an uncontrolled manner and may invade other tissues and parts of the body through the blood and lymph system. Cancer can take years, or sometimes decades to develop.
In the United States, one in four people develops cancer at some point in their lives. A cancer diagnosis can have devastating effects on the patient, their families, and the greater community. With the rates of cancer expected to increase, its burden on society, in terms of lost productivity, and costs of treatment and care, will exacerbate.
Extensive research has shown that the risk of cancer depends on a combination of multiple factors: behavioral, genetic and environmental. Anything that increases the chance of developing cancer is called a cancer risk factor. There are also some factors that play a protective role in cancer development. Some of these factors are modifiable or controllable, while others are not. For instance, smoking cigarettes is a modifiable risk factor as a person can control their exposure.
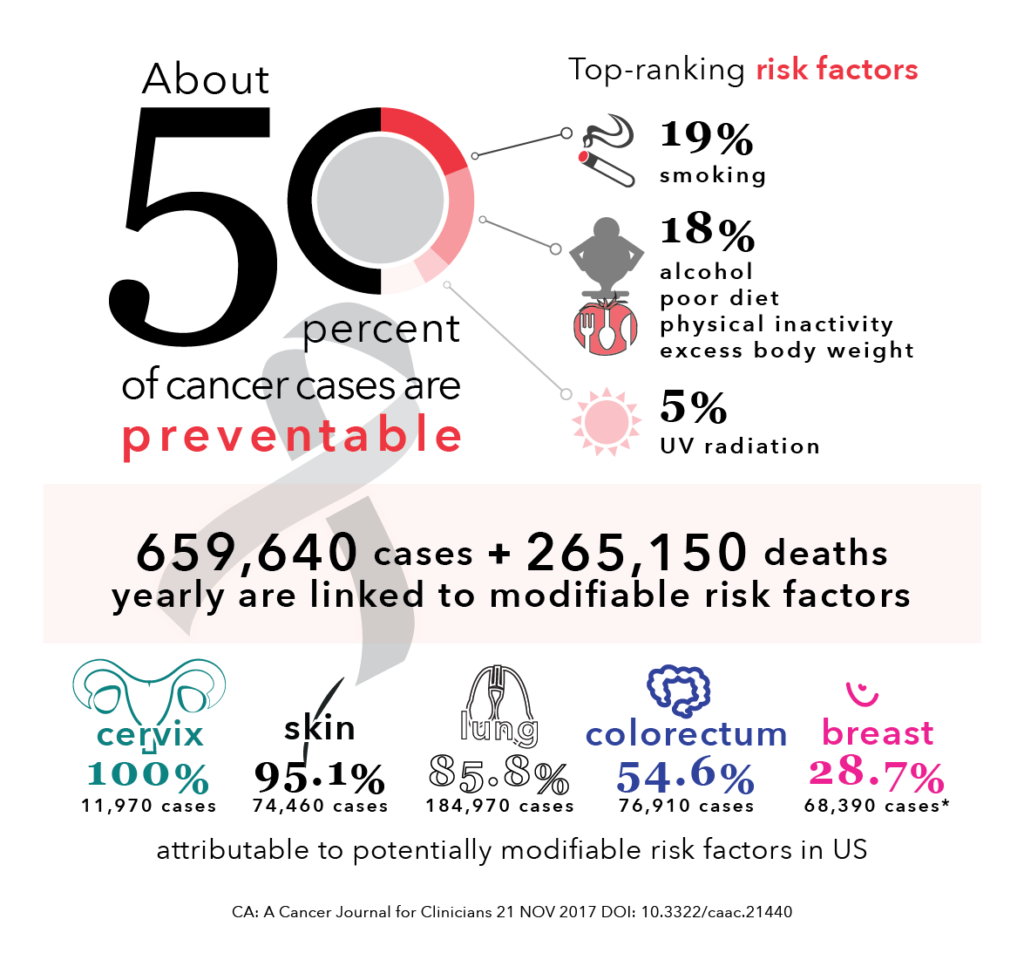
The American Institute for Cancer Research has reported that nearly 50% of common cancer cases are preventable [1]. Cancer prevention is any action taken to lower the chance of getting cancer. With the rates of cancer increasing, prevention is more important than ever to curtail cancer incidence. Primary prevention through behavioural interventions – commonly referred to as ‘lifestyle’ interventions – are the most cost-effective long-term strategy to reduce the burden of cancer and lower the number of deaths caused by cancer [2].
Here, we will review some major modifiable lifestyle factors that influence cancer risk. There are a set of factors that are known to increase the risk of cancer, such as:
1. Cigarette smoking and tobacco use
Tobacco is the single greatest controllable risk factor for cancer mortality, causing about 30% of all cancer deaths in the United States [3]. Tobacco use is associated with an increased risk of many different kinds of cancers, from bladder and cervical to esophageal and lung. A smoker’s risk of cancer, depending on how long a person has smoked, can be two to ten times higher than a non-smoker’s risk [4].
Exposure to second-hand smoke, also known as environmental tobacco smoke, also increases the risk of cancer and other diseases. The smoke that is exhaled by smokers or created through the burning of tobacco products contains the same cancer-causing chemicals as those inhaled by smokers. Recent evidence has also shown that residual nicotine and other chemicals left on indoor surfaces by tobacco smoke, known as thirdhand smoke, is hazardous and contains
Not smoking or quitting smoking dramatically lowers the risk of cancer diagnosis and death. People of all ages can improve their health by quitting smoking. People who quit smoking decrease their risk of lung cancer by over 30% after 10 years, compared to smokers. The risk of mouth or esophagus cancer is cut in half within 5 years after quitting [5].
For cancer survivors, the effects of smoking are even worse: there is an increased risk of cancer recurrence and negative long-term side effects from cancer treatment. Electronic software tools, such as EQUICARE CS™ (ECS), can facilitate this process by providing lung cancer screening forms and guidance to smoking cessation aids.
2. Radiation
There are two main types of radiation that are associated with an increased risk of cancer: ultraviolet (UV) and ionizing radiation. Ultraviolet (UV) radiation from sunlight is the main cause of nonmelanoma skin cancers. UV-emitting tanning beds have also been classified as carcinogenic. Sunscreen and protective clothing are effective preventive measures.
Ionizing radiation is released from medical radiation tests (e.g., x-rays and CT scan) and radon gas present in
3. Infections
There are certain infectious agents (viruses and bacteria) that are cancer-causing. In 2012, approximately 15% of all cancers were attributable to infectious agents [6]. These viruses and bacteria include:
- Human papillomavirus (HPV) that increases the risk for cancers of the cervix, penis, vagina, anus, and oropharynx
- Hepatitis B and hepatitis C viruses that increase the risk for liver cancer
- Helicobacter pylori that increases the risk of gastric cancer
Vaccines have been developed, and approved by the Food and Drug Administration, for the prevention of two of these cancer-causing agents: hepatitis B virus and human papillomavirus (HPV). These two vaccines can
Conversely, there are factors that may affect the risk of cancer. Nearly all of the evidence linking these factors to cancer risk come from observational studies. Data from observational studies is powerful as it gives researchers insight about relationships between potential factors and cancer risk. However, such studies cannot definitely establish a cause-and-effect relationship as their influence is complex and multifaceted. These modifiable factors include:
1.Alcohol
The harmful use of alcohol is a serious health
2. Physical activity
Physical activity includes any action that requires more energy than resting – working, exercising, and leisure activities. It is essential to maintain a balance between the calories consumed and used. There is substantial evidence that physical inactivity is linked to higher risks of several cancers [8].
The association between colon cancer and physical activity has been extensively studied. It has been found that most physically active individuals have a 24% lower risk of colon cancer, compared to those who were the least physically active [9]. With regards to breast cancer, many studies show that physically active women have a lower risk of breast cancer than inactive women. A meta-analysis has shown that the average breast cancer risk reduction associated with physical activity was 12%.
Physical activity has a number of biological effects on the body that help to explain associations with specific cancers. For instance, exercise can lower hormone levels and certain growth facts that are associated with cancer development and progression. Exercise can lower the risk of 13 specific types of cancer. There are also beneficial effects for several aspects of cancer survivorship [10], such as weight gain, quality of life, cancer recurrence or progression, and prognosis. [MD16] The American Cancer Society recommends that adults get at least 150 minutes of moderate intensity or 75 minutes of vigorous activity each week. [11]
3. Diet
The link between diet and cancer is as cryptic as the disease itself. For years, research has pinpointed certain foods and nutrients that
- Processed meat is any meat that has been smoked or fermented or includes added salts and nitrites – associated with an increased risk of cancer.
- Glycemic index (GI), a measure of how fast carbohydrates turn into sugar in the blood, can help identify
the whether certain carbohydrates are protective or detrimental for health. Consuming foods with a high GI (sugary drinks and processed foods) is associated with an increased risk of prostate cancer [12]. Conversely, eating lower-GI foods, such as legumes, with associated with a 30% lower risk of both prostate and colorectal cancers. - Antioxidants play an important role
for cancer prevention since assist in neutralizing free radicals that can damage cells. - Calcium may be a protective or a risk factor for certain cancers.
Some of these strategies mentioned are an effective alternative for preventing a larger burden of chronic disease worldwide, including cancer. Exposure to these factors is preventable. Through reducing exposure to these modifiable risk factors, 694,000 cases of cancer could be prevented in the United States every year [13]. It is important to note that there are things that can be done today to help prevent, delay, or even stop the cancer process.
Written by Dorri Mahdaviani , who holds a Masters of Public Health (MPH) from the University of British Columbia (UBC). Her academic and professional interests include the areas of chronic illnesses, health care systems and childhood health and development.
Infographics and Design by Ann Wong, who holds a PhD in Biochemistry and Molecular Biology from the Faculty of Medicine at the University of British Columbia (UBC), Canada. She is an author of over 10 SCI publications, having taught at UBC and the Peking University Health Science Center (PUHSC) in Beijing