EMR’s: So Many, So Expensive, and So VERY Confusing
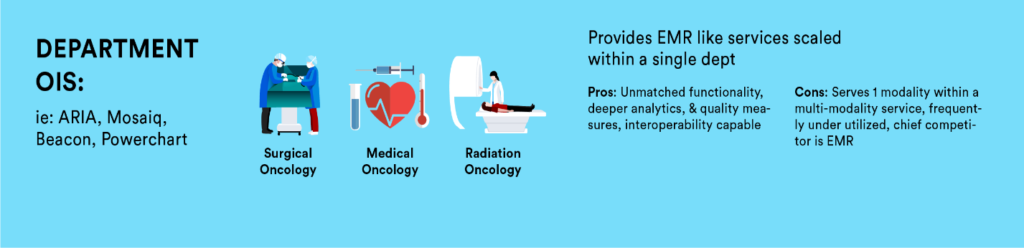
During our own professional careers, we have observed the rapid development of Electronic Medical Records (EMR) at various levels; from the wide enterprise level EMRs (Epic/Cerner/Athena/Meditech) that reach across hospitals and health systems to more specialized software that resides at a department level (ARIA/MOSAIQ/Beacon) and those even more granular at a functional level (Equicare/PACs/PowerPath) that provides specialized functionality not provided in other levels. Selecting a software involves a large range of influencers: CEO/CFO/CIO/Service Line Administrators, Department Director, clinical staff, physicians, nurses, and other ancillary staff with each having their own requirements influencing their choice. This complexity contributes to a somewhat less than ideal EMR infrastructure.
What does each individual care about? For a CFO, the cost savings associated with consolidation to a single enterprise level EMR is clear. For a CIO, an enterprise level EMR means fewer applications to manage, fewer resources to support, while also decreasing the risk for cyber vulnerability and record loss. Clinicians value the specificity to software while also the availability of information with fewer applications. Administration values reliability, availability of analytics/data, user satisfaction, costs, and other factors. In the end, no single person fully owns the outcome as there are numerous influencers and decision makers that weigh in with various and even competing expectations.
Enterprise level EMRs offer an opportunity to consolidate patient-related information into one centralized database. This alone is highly attractive as it provides a single source, high-level view of patient, clinical and financial information. Department-specific software provides functionality that enterprise level EMRs are simply incapable of, e.g. ARIA and Mosaiq. Both evolved from FDA approved Record and Verify systems that drove linear accelerators to become full departmental level information systems incorporating all treatment related activities that take place for a patient, such as: treatment schedules, simulation workup, treatment plan, billing, and consult/nurse documentation. As clinical care has become increasingly subspecialized, so have the tools to effectively manage. Functional level software is designed specifically to meet this increasingly complex demand that department and enterprise level are unable. For examples, a PowerPath software is necessary for tissue analysis while Equicare delivers end-to-end cancer care coordination including: interactive patient communication, screening, education, treatment summaries, and a comprehensive follow up plans. All of which are necessary when managing a chronic disease like cancer with efficiency and specificity. The value increases as we move away from a fee-for- service model and become more value based. This leaves us as oncology leaders to ask… what software do I really need to meet our goal of coordinating care for our patients and providing value-based care to our patients?

Rather than developing a comprehensive software plan that achieves our goals across departments, service lines, and even hospital networks, we often tackle software in silos not realizing the possibilities. Correcting this involves weighing the ambitions and vision of the organization with the financial expense, sensitivity to cyber security, and accepting the pain of implementing a software application plan.

The argument to consolidate and migrate all information to one enterprise level EMR offers great value on the surface. The issue with this, however, is that the scope of an enterprise level EMR is rather limited as no single EMR provides enough specificity to support and manage a complex service like oncology. The number of ongoing regulation and accreditation changes alone which must be kept current often creates a choice in labor intensive/inaccurate data or automated/accuracy. Our software tools provide the infrastructure we use to deliver care to our patients, yet we spend little time designing our platform. Most software applications do a good job within their scope and level; however, issues often arise when software is procured to do more than it is capable. Within our oncology space, this is a common occurrence. We should accept that this is less a fault of the software and more a fault of the organization implementing the software, as we are often asked and/or we attempt to utilize the wrong tool.
Here is an important factor to consider: once you have your software in place as designed, you are not done. You have consolidated in some areas and may add in others, need to address cyber threats, improved work flows, upgraded as entitled in service agreements, but still you have silo’d services. Everything we do in healthcare involves collaborating across services (adjuvant therapy). As our patients travel through the organization, our software should provide the infrastructure for their specific information to travel with them by being easily accessible to other care providers. This is only achieved via interoperability or establishing interfaces. When weighing software, value those that offer information exchanges with each other. Enterprise level EMR’s can offer bi-directional information exchanges with department level as well as specialized functional software. Not all information needs to convey, only what makes sense for patients, supportive services, providers and their referring network. Many software providers already have experience in identifying what data information is in demand, which is why they likely offer standard interface packages. Note, this serves as a starting point as each facility needs to identify what data they want to travel vertically and if up, down, or bi-directional. Additionally, you may need to specifically ask for the interoperability as the software provider likely prefers a consolidation to their own product or is not vested in an integrated solution ultimately serving our patients and network of providers.

Professional Opportunity
Within your organization, consider leading an initiative to organize your software so that it is aligned to the goals of your organization vertically. Ensuring it delivers horizontally within oncology on meeting security standards, reduces data-entry error/duplication, improved work flows for clinicians, access to data for analysis, accurate billing, timely scheduling, provides quality care coordination, patient education, data for accreditations, Patient Reported Outcomes (PROs), screening and long term Follow up plans. With senior leadership support, establish a small committee comprised of a representative from IT&S, clinical support, administration, fiscal/billing, quality, and risk management to drive the project. Below is a short list of suggested steps to begin with:
- Set a comprehensive goal for delivering end-to-end cancer services:
- Security (meets recognized standards)
- Functionality (comprehensive care coordination from screening through survivorship)
- Interoperability (create connectivity between functional, department specific, ancillary and enterprise wide EMR’s)
- How many software applications do you operate within your service line?
- List them and the functions you utilize as well as functionality not utilized
- Are your current applications HL7 compliant?
- Identify duplication
- Are you due for upgrades per a service agreement that would enable additional functionality?
- Identify redundancy where either toggling between or re-entering data
- Review contract terms to determine if owed upgrades, training, and out clause.
- Determine if you can consolidate?
- What do you utilize one for that another can do, maybe not do as well, but meets a standard? Consider the cost of errors if you plan to expose yourself to a manual process over an automated one, as well as the staffing resources for duplicate entry.
- Are you remaining current with your upgrades and would newest versions provide additional functionality?
- Is there a gap in what you have that cannot be made with existing software?
- Do you have IT&S staff who understand the products and have relationship with the vendors?
- Consider the safety implications of a patient presenting at an ER if the upstream EMR cannot adequately display what the patient’s previous treatment regimen has been.
- Is your IT&S staff capable of testing and implementing the required interfaces.
- What opportunities are there for bi-directional information exchanges through a set of standard interfaces?
- Can cost be bundled into purchase agreements?
- Can cost be amortized?
- Is it a capital or operational expense?
When you have selected the software design that supports your goals, work towards them understanding it will take time while remembering the value of integrated software applications. Existing contracts do not limit our ability, only the timeline and you may find you are owed upgrades and training. Do not simply purchase the cheapest software or the “best” software; rather, take time to identify what software is best for your organization given the level where it will reside with others along the vertical environment.
Summary
When a cancer program offers true care coordination across the service line, a byproduct is reduction in duplication, data-entry errors, missed billing, less toggling, better engagement between physicians-patients-departments, less volume leakage, more efficient passage through services, reduced cyber threats, increased staff capacity, adherence to Evidenced Based Guidelines (EBG), Patient Reported Outcomes (PRO), and a more streamlined patient centric approach. Regardless of what level the software resides at, the selection should not be a decision made in a vacuum. Rather, a multi-year strategic plan that leads to an agreed upon goal while understanding the value of leveraging your software together through information exchanges and interfaces.
In the end, providing comprehensive end to end cancer services that integrate with all EMR levels to deliver evidenced based guidelines, gain efficiency through automation and increases synergy between service lines, should be our goal. This means your functional software solution should coordinate patient care beginning with screening, managing the workup phase, seamlessly connect to multi-modality treatment care, inpatient/outpatient care, registration(s), billing, portal, and smoothly transitioning a patient through survivorship. Ideally, care coordination software will do all this and exchange the meaningful information with horizontal enterprise level EMR’s, ancillary support tools, i.e. pathology, radiology, etc… as well as department specific support tools, i.e. radiation, medical and surgical oncology information systems. Remember the winner is not the software that does it best, the winner is the patient with a SW that does interoperability both vertically and horizontally the best.
By: Steven Castle, MBA, RT(T)